Use of bioengineered human acellular vessels to treat traumatic injuries in the Ukraine–Russia conflict
Oleksandr Sokolov,a Vasyl Shaprynskyi,b Oleh Skupyy,c Oleksandr Stanko,d Serhii Yurets,c Yuliya Yurkova,e and Laura E. Niklasone,∗
aDnipro State Medical University, Dnipro, Ukraine
bState Institution of Science Research and Practical Center of Preventive and Clinical Medicine, Kyiv, Ukraine
cVinnytsya Regional Clinical Hospital, Vinnytsya, Ukraine
dOdessa Regional Clinical Hospital, Odessa, Ukraine
eHumacyte Global, Inc., NC, USA
On February 24th 2022, the Russian Federation invaded
Ukraine. Consistent with other modern conflicts, blasts
and shrapnel penetration have caused a large fraction of
the traumatic injuries, creating contaminated wounds
that often compromise the vascular supply to limbs and
organs. Although autogenous veins are the preferred
option for repair, their limited availability leads to the use
of synthetic grafts. However, usage of synthetic vascular
grafts carries a high risk of infection, meaning that there
is a lack of suitable conduit in some war-injured patients.
Human Acellular Vessels (HAVs) are bioengineered
vascular conduits that are cultured from human donors’
smooth muscle cells and subsequently decellularized.1 The
HAV is an investigational biological product in late-stage
clinical development, with over 1,000 patient-years of
exposure. After clinical implantation, the HAV repopulates
with cells, producing a living vascular tissue that may be
highly resistant to infection.2,3 In March 2022, surgeons in
Ukraine requested the HAV for vascular repair under
Humanitarian conditions. In response, the manufacturer
of the HAV (Humacyte Global Inc.) worked with the International Office of the US FDA and the Ukrainian Ministry of Health to provide HAVs to five hospitals in Ukraine.
Surgeons in Ukraine were trained remotely, by video
conferencing, on the procedures applicable to the HAV.
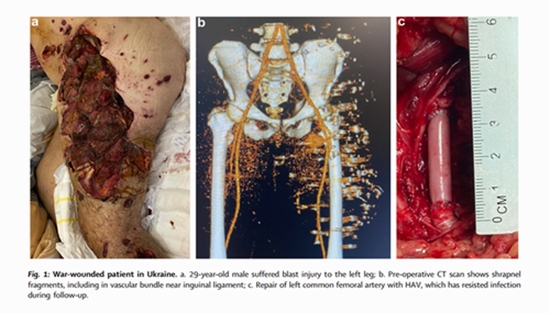
Since June 2022, 13 patients who lacked autologous
vein for repair have been treated with the HAV to repair a
range of arteries including superficial femoral, common
femoral, popliteal, and brachial arteries. Of these, 11 sustained limb vascular injuries in the ongoing conflict, mostly
comprising blast and shrapnel wounds. One such patient is
shown in Fig. 1, who underwent repair of the common
femoral artery on day 1, had patency of the HAV confirmed
at day 52, and who began ambulating on day 119.
Three patients received HAVs after failure of either
saphenous vein (n = 2) or synthetic graft (n = 1) to repair an
arterial injury. As of January 29th 2023, all HAVs retained
primary patency, and no infections nor amputations of the
affected limbs were reported. After follow-up times ranging
from 1 to 7 months, there have been no reports of HAV
conduit infection or mechanical failure. The Ukraine
real-world trauma experience demonstrates the potential
for regenerative medicine technologies to improve patient
outcomes in resource-limited environments.





ارسال نظر